Do you ever experience itching, irritation, or dryness in your vulvar area? The vulva, which includes the labia majora and labia minora, is a sensitive part of the body that requires proper care.
Thank you for reading this post, don't forget to subscribe!This guide will highlight common vulvar problems and offer easy tips to manage them. Keep reading to keep your vulvar health in check!
Key Takeaways
- Vulvar health involves proper care, gentle cleansing, and wearing breathable cotton underwear to reduce irritation and infections. Avoid douching as it can disrupt the vagina’s natural balance.
- Common vulvar conditions include yeast infections, genital herpes, lichen sclerosus, vulvodynia (chronic pain), and squamous cell carcinoma of the vulva. Early detection improves outcomes for serious concerns like cancer.
- Moisturizers like coconut oil or vitamin E can soothe irritation while water-based lubricants help with dryness during intimacy. Avoid petroleum jelly or fragranced products to prevent further issues.
- Regular check-ups play a key role in detecting STIs, HPV risks linked to vulvar cancer, or recurring problems like BV. Using probiotics and staying hydrated may also support healthy mucous membranes.
- Simple hygiene tips include wiping front-to-back after using the toilet and washing with lukewarm water only—no harsh soaps—to protect sensitive skin in areas such as the labia majora and minora.
Understanding Vulvar Anatomy
The vulva includes several parts that work together. These parts are the labia majora (outer lips), labia minora (inner lips), clitoris, vaginal opening, mons pubis, vestibule, urethral opening, and perineum.
Each has a specific role in sexual health, urination, menstrual flow, and reproduction.
The clitoris is key to sexual pleasure due to its many nerve endings. The labia protect sensitive areas like the vaginal introitus and urethra from bacteria or injury. The mons pubis provides padding for the pubic bone during physical activities or intercourse.
Together these features support overall vulvovaginal health while ensuring protection and functionality for women’s reproductive systems.
Common Vulvar Conditions
The vulva can face a range of issues that affect health and comfort. From skin changes to infections, each condition needs proper care for relief.
Vulvar skin complaints
Skin conditions like eczema, dermatitis, psoriasis, lichen sclerosus, and lichen planus often affect vulvar health. Dermatitis causes itching and rashes. It can be treated with corticosteroid creams or antihistamines.
Psoriasis leads to scaly patches and redness. Steroid creams or tar-based treatments help manage symptoms.
Lichen sclerosus triggers tenderness, itching, and painful sex. Autoimmune disorders often link to this condition. Topical steroids reduce discomfort with proper use. Lichen planus may cause pain or bleeding during sexual activity and raises the risk of vulvar cancer.
This condition also responds well to steroid-based treatments.
Caring for your skin keeps you comfortable now—and protects your long-term health.
Vulvar infections
Yeast infections, like vulvovaginal candidiasis, are common. Candida yeast causes them and leads to itching, burning, and thick vaginal discharge. Antifungal creams or pills often treat it quickly.
About 10% of women deal with recurrent infections—four or more a year.
Genital herpes causes painful blisters around the female genitalia. It spreads through sexual activity and is managed with antiviral medications. Genital warts appear due to HPV infection and require treatments like freezing or chemicals.
The HPV vaccine helps prevent these cases significantly over time.
Chronic pain of the vulva
Chronic vulvar pain, or vulvodynia, affects many women. It lasts over three months and has no clear cause. About 4.2% of women report this condition. Common symptoms include burning, itching, and discomfort around the opening of the vagina.
Pain often worsens during sexual activity or using tampons.
Vestibulodynia is a related condition causing sharp pain with tight clothing or touch near the vaginal walls. This can link to fibromyalgia or pelvic floor muscle issues. 85% of women with this type of vulvar pain experience dyspareunia (pain during sex).
Treatment may involve physical therapy for pelvic muscles, medications, or lifestyle changes like wearing cotton underwear for relief.
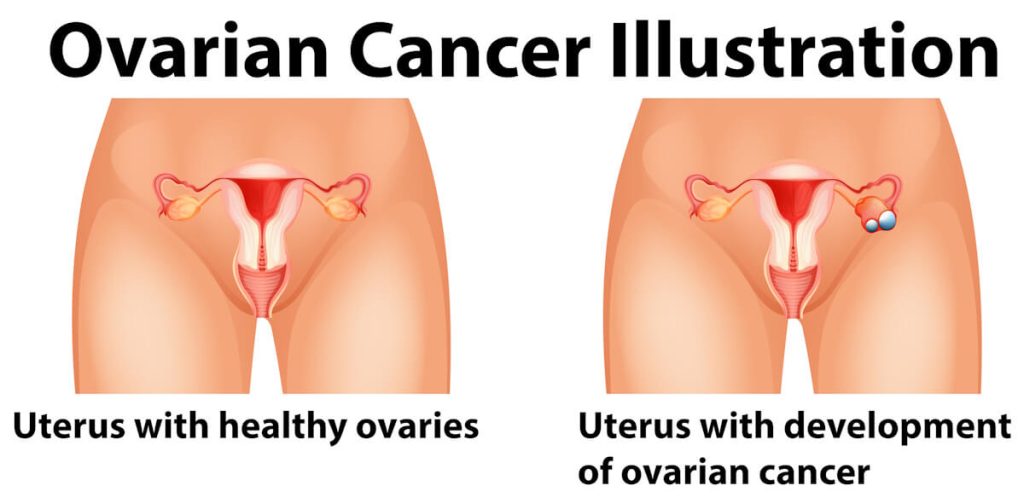
Cancerous conditions of the vulva
Squamous cell carcinoma makes up 90% of vulvar cancer cases. This type starts in the skin cells. Melanoma accounts for about 5%, beginning in pigment-producing cells. Adenocarcinoma is rare, under 1%, and forms in the Bartholin glands.
Vulvar cancer mostly affects older adults, with an average age of diagnosis at 65.
Human papillomavirus (HPV) infection increases the risk of squamous cell carcinoma of the vulva. Regular screenings can help spot issues early. Symptoms might include itching, pain during intercourse, or unusual growths near the vaginal area or labia majora and minora.
Early detection improves treatment outcomes significantly.
Best Practices for Vulvar Care
Taking care of the vulva supports comfort and health. Simple habits can reduce irritation, dryness, or infections—keeping this area clean and balanced matters.
Gentle cleansing
Keeping the vulva clean is key to good vulvar health. This helps prevent infections and irritation while maintaining a healthy balance.
- Wash the vulva daily with lukewarm water. Avoid hot water, as it can cause dryness or irritation.
- Use a soft washcloth for cleaning. Gently pat the area; don’t scrub too hard.
- Skip soaps directly on your vulva. Soap can disrupt the sensitive pH balance, which ranges between 3.5 to 4.7.
- Choose a pH-balanced feminine wash if needed. Make sure it’s free from strong fragrances or harsh chemicals.
- Rinse thoroughly after washing to remove any residue that may cause vaginal irritation.
- Pat dry using a clean, soft towel after washing, avoiding rough rubbing motions.
- Avoid using dryer sheets or fabric softeners on underwear, as these can irritate sensitive skin.
- Stick to breathable fabrics like cotton underwear to keep the area cool and dry throughout the day.
Proper wiping technique
Cleaning the vulva properly is vital for good vulvar health. Incorrect wiping can lead to infections and irritation.
- Always wipe front-to-back after using the toilet. This avoids spreading bacteria from the anus to the vaginal area.
- Use soft, unscented toilet paper to prevent vaginal irritation or sensitivity caused by harsh chemicals.
- Pat dry instead of rubbing the area. Rubbing can irritate delicate skin like the labia majora and labia minora.
- Cleanse the vulva gently after bowel movements if needed. This helps reduce contamination risks and keeps the area fresh.
- Avoid excessive wiping, as it can lead to redness or soreness in sensitive areas around your reproductive organs.
- Teach young girls proper wiping habits early to prevent urinary tract infections (UTIs) as they grow older.
- Consider using a bidet or moistened wipes (unscented and alcohol-free) for gentler cleaning during menstrual cycles or after sexual activity.
Wear breathable underwear
Choose cotton underwear for better vulvar health. Cotton allows airflow and absorbs moisture, reducing the risk of vaginal infections like yeast infections or bacterial vaginosis. Synthetic fabrics can trap heat and sweat, leading to irritation or vaginal itching.
Switching underwear daily keeps the area clean and dry. Wearing none at night can improve air circulation and prevent moisture buildup. This simple habit supports natural lubrication balance while lowering discomfort from vaginal dryness or irritation.
Avoid douching
Wearing breathable underwear helps maintain a healthy environment. But douching can undo this balance and harm vulvar health.
Douching disrupts the natural vaginal pH. This makes it easier for infections like yeast or bacterial vaginosis to develop. Studies show it also raises the risk of pelvic inflammatory disease (PID) and infertility.
The American College of Obstetrics and Gynecology warns against using these products. Trust your body’s cleaning process instead—your vagina already takes care of itself!
Managing Vulvar Discomfort
Caring for vulvar discomfort can include simple steps to ease itching, dryness, or irritation—read on for helpful tips.
Using non-hydrating (soothing) moisturizers
Natural oils like vitamin E and coconut oil can ease vulvar discomfort. These non-hydrating moisturizers help soothe irritation without adding extra moisture. Carlson KeyE Suppositories work well at bedtime for calming sensitive skin.
Stick to gentle options for vulvar skin care. Avoid products with fragrances or harsh chemicals that might cause vaginal irritation. Always check labels, ensuring safe ingredients for the labia majora and labia minora areas.
How to use vaginal and vulvar moisturizers
Using vaginal and vulvar moisturizers can help reduce dryness and discomfort. Follow these steps for safe and effective use:
- Wash your hands before applying any product to avoid introducing bacteria. Clean hands reduce the risk of infections.
- Choose a trusted brand like HYALO GYN, Revaree, Replens, or Good Clean Love. These are specially designed for hydration without irritation.
- Apply at bedtime for better absorption while your body is resting. Nighttime use allows the product to work longer.
- Use the moisturizer 3 to 5 times a week for consistent results. Regular application helps maintain hydration over time.
- Avoid petroleum jelly as it may cause allergic reactions or trap bacteria. Stick with safe, water-based options.
- Squeeze the recommended amount onto clean fingers or an applicator device if provided. Follow the instructions on the label carefully.
- Spread the product gently around the vulva or inside the vaginal canal as directed on packaging instructions.
- Wear breathable cotton underwear after applying to keep air circulating and prevent irritation.
- Store products in a cool, dry spot away from direct sunlight to preserve their quality.
- Replace expired moisturizers promptly, as outdated products lose their effectiveness and may irritate skin.
Vaginal lubricants and their applications
Vaginal lubricants play a key role in managing vaginal dryness and enhancing sexual activity. They reduce friction, making intimacy more comfortable and enjoyable.
- Water-based lubricants are often the best choice. They cause less vaginal irritation and are easy to clean up after use. Brands like KY Jelly or Astroglide offer great options.
- Silicone-based lubricants provide longer-lasting effects. Options such as Pjur or Uberlube are ideal for people who need extra moisture during sexual contact. They work well even underwater, like in showers or baths.
- Avoid oil-based products if using condoms. Oils weaken latex, increasing the risk of sexually transmitted infections (STIs) and unplanned pregnancies.
- Consider personal needs while selecting lubricants. Those with sensitive skin may prefer hypoallergenic formulas without perfumes or dyes.
- Use coconut oil carefully as a natural alternative. It works for some but can cause irritation in others and might not be safe with barrier contraceptives.
- Lubricants help prevent pain or discomfort during sexual activity caused by vaginal atrophy, which sometimes occurs after menopause.
- Apply lubricants directly to the genital area or sex toys before use for smooth application and impact where needed most.
- Pair water-based options with safer sex practices like barrier methods to lower risks of STIs during intimacy effectively.

Preventative Measures and Regular Care
Take small steps daily to keep your vulvar health in check. Stay proactive about care to avoid discomfort or infections.
Regular check-ups
Regular check-ups help maintain vulvar health and catch issues early. They allow doctors to spot signs of vaginal infections, sexually transmitted infections (STIs), or other concerns like genital warts or human papillomavirus (HPV).
These visits also provide a safe space to discuss vaginal dryness, irritation, or abnormal discharge.
Healthcare providers can educate women on proper vulvar care during these appointments. Routine screenings for STIs and assessments of sexual health ensure long-term wellness. Making regular exams part of your routine supports overall genital health and peace of mind.
Consider probiotics
Probiotics may support vaginal health by restoring balance to the female reproductive system. The L. acidophilus strain might help prevent or manage conditions like bacterial vaginosis (BV).
Including yogurt with live cultures in your diet is a simple way to get probiotics.
These “good bacteria” can reduce vaginal irritation and improve vulvovaginal health. They may also help reduce risks of yeast infections and other imbalances affecting the labia majora or minora.
Probiotic-rich foods like kimchi, kefir, or sauerkraut are tasty options for maintaining a healthy microbiome.
Stay hydrated
Drinking plenty of water helps keep mucous membranes in the vaginal area healthy. Proper hydration reduces the risk of dryness and supports overall vulvar health. Aim for at least eight glasses a day to meet your body’s needs.
Staying hydrated can also lower the chances of urinary tract infections (UTIs). Water flushes toxins from the body, keeping bacteria under control. If you experience vaginal irritation or dryness during sexual activity, better hydration might help ease discomfort.
Conclusion
Caring for vulvar health keeps you comfortable and confident. Simple habits like wearing cotton underwear, using gentle cleansers, and avoiding harsh chemicals make a big difference.
If issues arise—like itching or irritation—seek professional help rather than guessing. Regular check-ups and proper hygiene protect against infections and discomfort. Your vulva deserves attention, care, and kindness every day!
For insights into other health considerations, explore our deep dive on the risks and realities of waist training.
